- How are they diagnosed?
- Is imaging helpful in making this diagnosis?
- How are moles treated? Will I need a hysterectomy?
- How does this diagnosis impact a pregnant woman? Will my baby survive?
- Can I have children after being diagnosed with this?
- How curable is this?
- How is it staged?
- How is it treated?
- What happens if GTN does not go in to remission or returns?
Gestational trophoblastic neoplasia (GTN) constitutes a very rare group of tumors that can grow from cells inside a woman’s uterus. Unlike endometrial cancer, which arises from the lining of the uterus called the endometrium, GTN arises from the cells that normally make a placenta (afterbirth) during a pregnancy. Trophoblast refers to the specialized cells that normally surround an embryo. These cells ultimately will make the placenta that will feed the fetus during the pregnancy. Sometimes the fertilization process is abnormal and, instead of a normal pregnancy, a “molar pregnancy” results from abnormal development of the trophoblast.
This abnormal pregnancy can be a “complete mole” meaning that it consists of all trophoblast and no fetus, or a “partial mole” meaning that there is also fetal tissue present. This fetal tissue is always abnormal because the partial mole is “triploid”—has three sets of DNA chromosomes rather than the normal two. A complete hydatidiform mole most often develops when either 1 or 2 sperm cells fertilize an “empty” egg cell (a cell that contains no nucleus or DNA). All the genes come from the sperm cell. These moles are usually XX. A partial mole occurs when two sperm fertilize a normal egg. All partial moles are “triploid” for this reason: XXY or XYY.
A complete mole can metastasize (spread). The molar pregnancy can invade into the uterus and can spread to distant organs, usually liver or lungs. Even with spread, most molar pregnancies can be cured.
Beyond molar pregnancies, there are two other types of GTN. Choriocarcinoma is a very aggressive form that usually develops after a complete mole, but rarely can be seen after a partial mole or even a normal pregnancy. It has the propensity to metastasize early. Placental site trophoblastic tumor (PSTT) develops from the place where the placenta attaches to the endometrium. The PSTT can invade into the uterus and be very difficult to treat medically. As such, it is the only GTN where a hysterectomy may be necessitated in order to effect a cure.

As noted, these are exceedingly rare events. About 1 in every 1,500–2,000 pregnancies in the United States is a molar pregnancy. The incidence is higher in Asia for unclear reasons, affecting 1 in 120 pregnancies in that area of the world. Invasive moles affect 1 in 15,000 pregnancies and choriocarcinomas affect 1 in 40,000. Complicated twin gestations where a viable fetus co-exists with a mole is exceedingly rare, seen in 1 in 22,000–100,000 pregnancies.
There are risk factors associated with GTN:
- Women under 20 and over 40
- Prior history of a molar pregnancy
- Prior miscarriages
- Being A-positive or AB-positive blood type
Trophoblast
Specialized cells that normally surround an embryo and ultimately make the placenta that will feed the fetus during the pregnancy.Molar pregnancy
Pregnancy that results from abnormal development of the trophoblast.Hydatidiform mole
The result that most often develops when either one or two sperm cells fertilize an “empty” egg cell (a cell that contains no nucleus or DNA).Choriocarcinoma
A very aggressive form of GTN that usually develops after a complete mole, but rarely can be seen after a partial mole or even a normal pregnancy.Placental site trophoblastic tumor (PSTT)
A tumor that develops from the place where the placenta attaches to the endometrium.
How are they diagnosed?
In GTN, the blood pregnancy test, which measures human chorionic gonadotropin (or hCG) will be extremely elevated, often much higher than what would be expected normally. In addition, the hCG does not follow the normal pattern of expression one sees in pregnancy or else, in the woman who has delivered a baby or had loss of the pregnancy, it fails to return to normal.
Beyond that, women with a complete mole may have the following signs and symptoms during the first trimester of pregnancy:
- Vaginal bleeding
- Ovarian cysts
- Uterine size that is larger than expected based on lastmenstrual period
- Severe nausea and vomiting
- High blood pressure very early in pregnancy
- Signs of hyperthyroidism
Similar symptoms may be seen with the other forms of GTN as well. Partial moles usually present with abnormal bleeding in the context of a pregnancy. In such cases, it would be important to rule out a miscarriage. Women with choriocarcinomas may present either as part of a missed abortion picture or after delivery of an abnormal or normal pregnancy.
It is important to note that, while the hCG is an indicator of GTN, it can also be falsely elevated. That is, the hCG test can be abnormal and you be not pregnant or have a mole. This situation is referred to as a “phantom hCG”. This can happen because your body may have proteins that are interfering with the way the lab tests for hCG, usually because proteins are reacting to the test. If the hCG is the only evidence of a problem, it must be repeated.Your doctor can even test for it in your urine. In phantom hCG, the level is usually normal.
In addition, there are special reference laboratories that can check your blood for any factors that may cause this abnormal report. The importance of recognizing phantom hCG is that women have been misdiagnosed with GTN and gone through chemotherapy inappropriately. Knowing whether the hCG is a real result or is false will hopefully prevent women from being exposed to chemotherapy that is not needed.
Is imaging helpful in making this diagnosis?
Ultrasound is very sensitive and reliable for diagnosing both complete and partial moles. An ultrasound will reveal a “snowstorm” pattern inside the uterus and, in cases of a complete mole, there will be no evidence of a fetal heartbeat or fetal parts. There may also be evidence of many ovarian cysts, which can be associated with complete mole. The presence of a fetus supports the diagnosis of a partial mole.
Women with PSTT may have an abnormal lesion identified by ultrasound. Alternatively, it may appear to be an area of abnormal signaling on ultrasound, called echogenic foci, surrounded by areas consistent with blood, called hemorrhagic cysts. If taken in the context of a pregnancy or as new onset bleeding in a woman who has already delivered her baby, this diagnosis should be ruled out.
How are moles treated? Will I need a hysterectomy?
Both complete and partial moles are treated with a D&C to empty the uterus. Prior to the procedure, your doctor will check a chest x-ray to make sure that there is no evidence of disease in the chest. Your doctor will also check to make sure your thyroid function is normal, that your blood chemistry is normal, and that you are not significantly anemic as these factors may complicate your procedure.
The cervix is dilated (opened) and the contents of the uterus are completely removed. Looking at the tissue under the microscope makes the diagnosis of a complete or partial mole. It is important to stress that there is usually no viable fetus present in either of these diagnoses.
In most cases a hysterectomy is not required. After the procedure, the doctor will check blood tests to make sure the pregnancy blood test numbers come back to normal.
Only in the case of PSTT, which is very rare, may a hysterectomy be needed.
How does this diagnosis impact a pregnant woman? Will my baby survive?
In complete moles, there is no baby present; in partial moles, the fetus is usually malformed or appears inappropriate for the expected age, or is usually not present at all, though fetal parts can be identified on ultrasound. In both cases, the fetus is not expected to go to term, let alone survive, and all cases end in a spontaneous abortion or miscarriage.
In extremely rare circumstances, a normal pregnancy may coexist with a mole. This situation is referred to as a “twin pregnancy.” There are fewer than 200 cases reported in the medical literature, and most are associated with the use of technology to have a baby, or assisted reproductive technologies.Twin pregnancies are a high-risk situation, and all cases should be referred to specialists in high-risk pregnancies (maternal fetal medicine) and to gynecologic oncologists.There is hope that your baby can survive even with a coexisting mole, but it is a very serious situation that requires input from specialists.
Can I have children after being diagnosed with this?
Most women diagnosed with a partial or complete mole will have a complete recovery with only a D&C. These women will almost certainly be able to conceive a nor-mal pregnancy following the diagnosis; however, they are at increased risk over the general population to have a second molar pregnancy. Therefore, it is recommended that women get an early ultrasound with subsequent pregnancies to exclude a recurrent mole.
Still, pregnancy is possible after the diagnosis of GTN; even after choriocarcinoma treatment, patients can still have normal pregnancies. For women with PSTT, if a hysterectomy has been done, then you will not be able to carry your own child; if the ovaries were spared, however, you could still undergo in vitro fertilization to create embryos, who can then be transferred to another woman (called a gestational surrogate) to carry for you.
How curable is this?
GTN is very curable. Partial and complete moles can be cured with surgery alone (D&C). If the hCG blood test remains elevated or rises, or if there is evidence of metastasis, chemotherapy is given. Chemotherapy is highly curative in this disease, even when there are metastases to the liver or lungs.
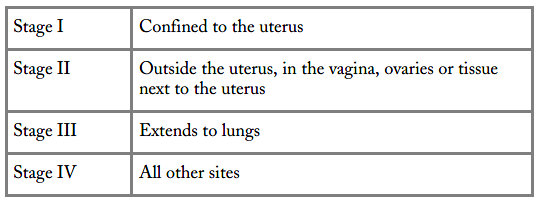
How is it staged?
There are two different staging systems for GTN. One is released by the International Federation of Obstetrics and Gynecology (FIGO). It describes the extent of disease spread. Notably, disease that has spread to lungs is considered as Stage III, whereas disease involving any other organ (like the liver or brain) is considered Stage IV. This reflects the different risks a woman faces with GTN and the fact that spread to the lungs is not as serious as having it go to other organs.
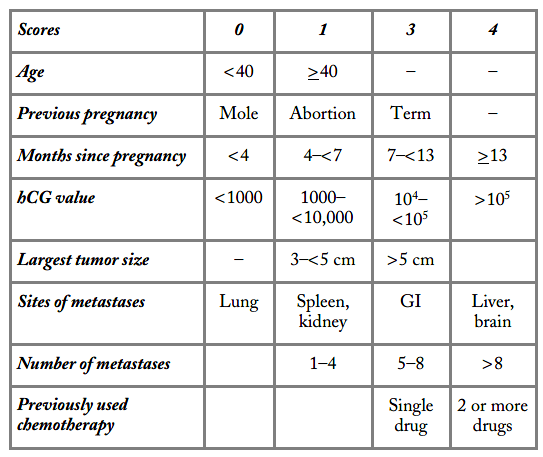
The other system is called the modified World Health Organization (WHO) scoring system. This system is used for women with persistent or metastatic disease to assist in choosing appropriate treatment.
 `
`
The “score” is calculated based on certain prognostic factors for having persistent disease. These include your age, whether a pregnancy was associated with it (and if so, the time that elapsed from the pregnancy to the diagnosis), areas of disease, and whether or not prior treatment was given. The important thing to know is that the score can change if the disease comes back. That is, even if you started out with one score, your doctor will re-do the scoring system if you relapse.
How is it treated?
Molar pregnancies are treated with D&C. The level of blood pregnancy test is then followed weekly until it is non-detectable. Sometimes there is persistent disease; this is diagnosed by a continued elevated blood pregnancy test. If that happens, it is assumed that there are still abnormal trophoblastic cells present. These can be treated with single agent therapy and either methotrexate or actinomycin-D is used. If you have choriocarcinoma, or if your WHO score is 7 or over, then you face a higher risk of relapsed disease.
In this case, more complicated regimens are used, such as etoposide, methotrexate and actinomycin-D (EMA) alternating with cyclophosphamide and vincristine (CO), also known as EMA-CO. For PSTT or persistent GTN despite EMA-CO, a variation is used where the EMA alternates with etoposide and cisplatin, known as EMA-EP. If you require chemotherapy beyond single agents, it is best to be seen by someone who is an expert in the management of GTN.
Etoposide is given by IV and works by blocking the function of the protein, topoisomerase, which is involved in stabilizing DNA. Its side effects are hair loss, diarrhea or constipation, a metallic taste that can develop, and lowering of blood counts. It also carries a risk of injury to the bone marrow and can cause leukemia later on in life.
Methotrexate blocks the folate pathway, an important vitamin pathway in the body that is involved in the creation of DNA and RNA. It too can affect the bone marrow, but may also have a negative effect on the gastrointestinal system. Patients receiving methotrexate can develop sores or ulcers all along their GI system from their mouth down the esophagus, and even involving the colon and rectum. It can also lead to liver inflammation general chemotherapy side effects including fatigue, lowering of blood counts, hair loss, and mouth sores.
Cyclophosphamide is a very old drug, available as an IV and oral (PO) formulation. For GTN, it is given IV. It is actually a pro-drug, which means it is converted to an anticancer drug after it enters the body. This conversion occurs in your liver. It causes the usual side effects of treatment, including nausea, vomiting, lowering of blood counts, hair thinning, and diarrhea. It can also be toxic to the bladder and may even result in bladder cancer as a future risk, but with proper fluid given during and after treatment, this risk can be minimized.
Vincristine works on dividing cells to lead them to death. It works similarly to paclitaxel and, like paclitaxel, it can cause numbness and tingling to develop. At its worst, it can cause a foot drop, which happens when you cannot turn the ankle and toes upward. You might complain that you have started to trip on your own feet as the first sign of this. Vincristine can also cause significant constipation due to its effects your doctor know about them before they get serious.
Your hCG will be followed every 10–14 days on treatment, and as long as it remains elevated you will require treatment. Once it normalizes 1-2 extra cycles are given, mostly as extra insurance. Once in remission, you will need to have this level checked regularly over the next
two years. You should also avoid pregnancy during this period of active follow-up. As long as the hCG is normal you should not require any further testing. However, if it starts a sustained rise (repeated twice with confirmed rises) you will need to be re-staged.
After treatment (especially with multi-agent chemotherapy) you will need to be followed for a long time, even if it is no longer with your oncologist.This is because there is a risk of a secondary cancer related to treatment, and the type of cancer risk changes the longer you are followed:
- There is a risk for leukemia up to 4 years after treatment.
- There is a risk for colon cancer between 5 and 9 years of follow-up.
- There is a risk for melanoma 10 to 14 years later.
- There is a risk for breast cancer 25 years after treatment.
Knowing these risks will be an important point to remember as you embark on follow-up as a cancer survivor.
What happens if GTN does not go in to remission or returns?
The risk of recurrence or progression has been associated with several factors:
- Liver involvement
- Brain involvement
- Detection of disease six months or longer from the prior pregnancy
- Term delivery
While it does not change the treatments you will receive, it is knowledge that will explain the surveillance you will need following treatment. Still, even women who have recurrent disease or disease that spreads can still be cured because GTN is very sensitive to chemotherapy. Metastatic disease is almost al-ways curable with single drug chemotherapy. High WHO score choriocarcinoma and invasive moles that have already seen one or two lines of treatment are harder to treat and require more complicated regimens.
If the tumor comes back even after multiple trials, surgery may be considered in an attempt for cure. How-ever, women do still die of this disease and if, after multiple treatments, the cancer comes back, a frank discussion on the benefits of further treatment will be required. Fortunately, this is rarely the case, but if it happens to you, seeking out a specialist who has seen lots of these cases should be strongly considered.